Diabetes Free SC (DFSC) launched in 2020 with a mission to reduce health care gaps and improve the health of all South Carolinians affected by diabetes. The program is a long-term commitment to transform the health of all South Carolinians by preventing diabetes and its complications in adults, reducing lifelong risk of diabetes in children and improving pregnancy outcomes in women with diabetes.
In October, DFSC developed two prenatal programs for women with diabetes. MOMs in Control is a combined effort between Prisma Health–Midlands and Carolina Diabetes and Kidney Center in Sumter. Its goal is to make access to care easier for mothers in that rural area. MOMs in Control of Diabetes Upstate, located in Greenville, is based in one of the largest obstetric practices in South Carolina.
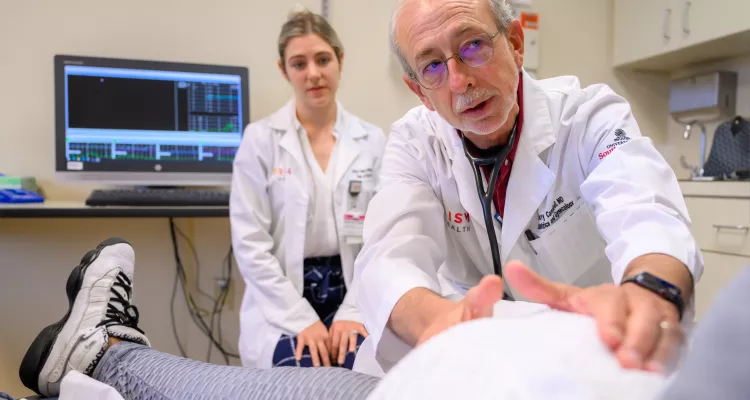
Each program offers care for pregnant women with diabetes through multidisciplinary prenatal clinics. These clinics combine the care of maternal fetal medicine specialists, endocrinologists, nutritionists, diabetes educators and patient navigators to provide team-based care. Currently, 300 women are participating in these programs.
Dr. Misti Leyva, administrator of the DFSC pregnancy initiative, says the multidisciplinary approach creates a “one-stop shop” that reduces the time, cost and energy demands on pregnant women. Leyva offers insights into why the prenatal programs are a key part of the DFSC initiative.
Why focus on pregnant women with diabetes?
Maternal and infant mortality rates in the United States are among the highest in the developed world. The highest rates in the nation are here in the Southeast. Rates of death in mothers and infants are three to four times higher in Black Southerners than in white Southerners. Black Southerners also have higher rates of diabetes and pre-diabetes. This is mainly because of disparities in social determinants of health. Maternal and infant mortality rates are doubled by pre-pregnancy diabetes. In fact, any degree of high glucose can lead to challenges in pregnancy.
Our strategy is founded on two important principles. First, there is clear evidence that establishing good health early in life reduces risk for diabetes and its complications for decades into the future. A pregnant woman and particularly her unborn child gain lifelong benefits from a well-managed pregnancy. Second, we appreciate the influence young mothers can have on multiple generations within their families and on society in general.
By working with a relatively limited population for a short but crucial time — those nine months of pregnancy — we create a highly effective, long-term strategy to combat diabetes.
What impact will improved pregnancy outcomes have on the prevalence of diabetes in South Carolina?
DFSC aims for statewide, population-level change. Diabetes inflicts silent damage over years and decades, but research shows early intervention can delay complications and prolong a healthy life. Our efforts to address diabetes in pregnancy is an example of the earliest possible intervention in the disease process.
Our hope in focusing medical care and education on young mothers is to create a ripple effect that extends beyond mothers and their babies and into their families and communities. We expect to see this improving the landscape of diabetes in South Carolina.
What will it take to keep the momentum going with children and with adults?
In addition to DFSC’s focus on improving pregnancy outcomes in women with diabetes, we focus on reducing lifelong risk of diabetes in children and preventing the disease and its complications in adults.
To make sure children across South Carolina can experience healthier school environments, DFSC supports two complementary organizations that focus on school-based wellness: the Alliance for a Healthier Generation and the Medical University of South Carolina Boeing Center for Children’s Wellness.
The overall goal of these programs is to increase opportunities for physical activity and healthy eating, reducing future risk of diabetes and other chronic diseases in adulthood. It’s more difficult to address diabetes in adults. DFSC’s initial response is to increase access to healthy foods through its support of FoodShare South Carolina, a program that works to increase access to fresh produce. Other programs to win the fight against diabetes are coming soon.

What results are you hoping to see regarding the health of mother and baby?
Poor control of diabetes during pregnancy increases the chances for almost every pregnancy problem for mother and baby. Only 20 percent of diabetic pregnancies in our state attain and maintain blood sugar in a healthy range — an A1C of less than 7 percent —throughout pregnancy.
Excessive weight gain during pregnancy also is linked to diabetes and leads to maternal and neonatal complications. Only 24 percent of pregnant Black women in South Carolina achieve recommended weight gain during their pregnancy. Coordinated care for pregnant women with diabetes will significantly increase the number who attain and maintain healthy blood sugar levels. It will also increase the number who achieve a healthy level of weight gain during pregnancy. We also hope these efforts will reduce the number of unplanned hospital admissions of pregnant women.
Why are multidisciplinary programs so important to improve pregnancy outcomes?
Best practice requires coordinated care — delivered by maternal-fetal medicine and diabetes specialists and supported by diabetes educators, nutritionists, ophthalmologists and behavioral health specialists working as a team. Ideally, this team is in one location at a “one-stop shop” and backed by community health workers. The alternative is separate visits to different providers that impose time, cost and energy demands that are impossible for many pregnant women, especially those living in low-income or rural communities.
Communication among providers also suffers when care is fragmented. Our MOMs programs aim to provide coordinated services at a single visit and location. This saves time, money, energy and stress for patients while providing comprehensive medical care for high-risk pregnancies.
This team-based care before babies are born is key to improving the state’s birth outcomes, meeting the needs of patients in the reality of their lives and reducing short- and long-term maternal and infant illness and death. This project unites team members who used to operate in isolation and improves value and efficiency by making it easier for them to communicate.
Clinic staff and administrators from participating clinical departments support each team. This model improves the coordinated care of the patient and reduces the stress of a high-risk pregnancy.